Introduction
When visiting a hospital or being admitted as a patient, you may come across various monitors that display a plethora of numbers, waveforms, and symbols. These monitors are essential for healthcare professionals to monitor your vital signs and detect any abnormalities in real-time.
Understanding how to read these hospital monitors can be overwhelming if you are unfamiliar with medical terminology and equipment. However, by familiarizing yourself with the basics, you can gain a better understanding of what these monitors are displaying and what they mean for your health.
In this article, we will delve into the different aspects of reading hospital monitors, including interpreting vital signs, analyzing waveforms, and understanding alarm notifications. By the end of this guide, you will have a clearer understanding of how to interpret the information displayed on these monitors and how it relates to your overall health and well-being.
It is important to note that while this guide provides valuable insights, it is not a substitute for professional medical advice. Always consult with healthcare professionals for accurate diagnosis and treatment.
Now, let’s dive into the fascinating world of hospital monitors and empower ourselves with the knowledge to decipher their valuable information.
Understanding Basic Vital Signs
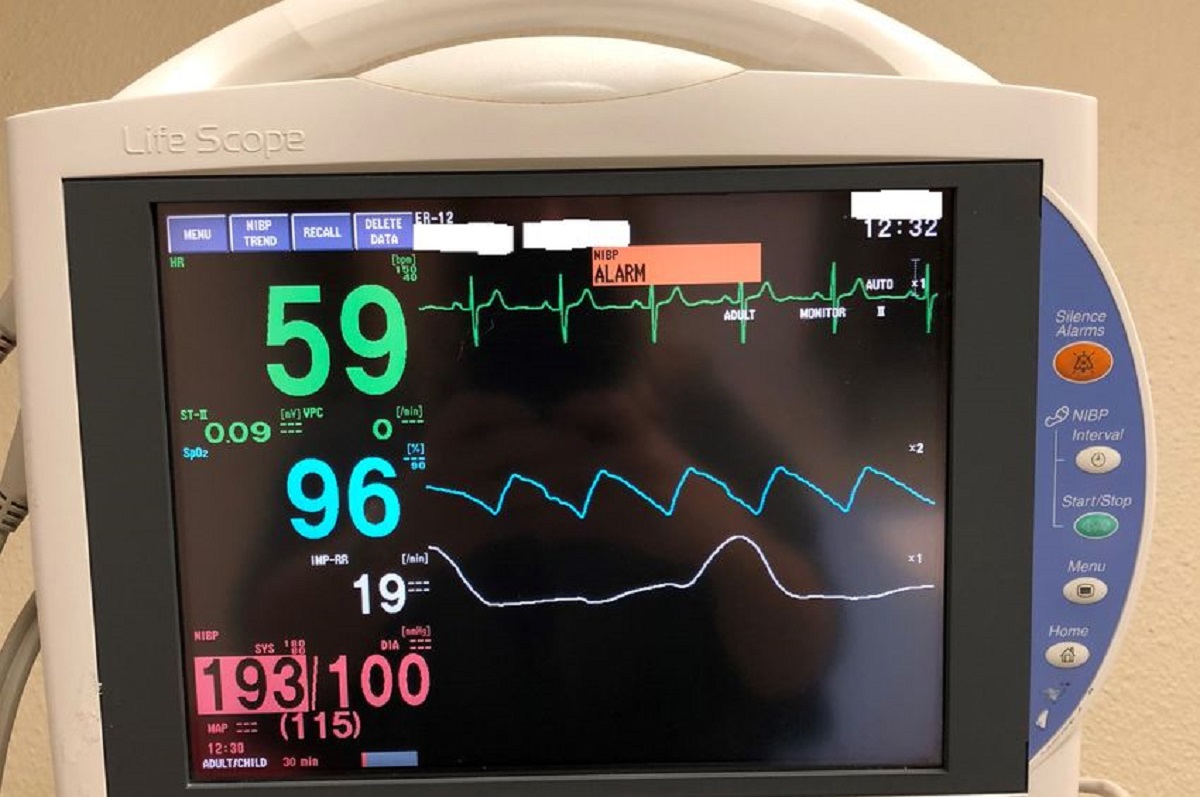
When reading a hospital monitor, the first and most crucial information you will encounter is the display of vital signs. These vital signs provide valuable insights into your overall health and help medical professionals assess your condition. The four basic vital signs are:
- 1. Blood Pressure: Blood pressure is measured in two numbers: systolic pressure (the top number) and diastolic pressure (the bottom number). It indicates the force of blood against the walls of your arteries. Normal blood pressure is generally around 120/80 mmHg.
- 2. Heart Rate: Heart rate, also known as pulse, refers to the number of times your heart beats per minute. A normal resting heart rate for adults ranges from 60 to 100 beats per minute.
- 3. Respiratory Rate: Respiratory rate represents the number of breaths you take per minute. The normal range for adults is typically 12 to 20 breaths per minute.
- 4. Temperature: Temperature is a measure of the body’s internal heat. It is usually measured in degrees Fahrenheit or Celsius. Normal body temperature ranges from 97.8°F to 99°F or 36.5°C to 37.2°C.
By monitoring these vital signs, healthcare professionals can quickly identify any abnormalities or deviations from the normal range, which can indicate underlying health issues or complications. It is important to note that individual factors, such as age, medical history, and current condition, can influence what is considered normal for each person.
Understanding and interpreting these vital signs is crucial for both medical professionals and patients. It can help detect early warning signs of various medical conditions, monitor the effectiveness of treatments, and identify potential complications.
Remember, vital signs are just one component of the overall picture of your health. They should be assessed in conjunction with other clinical information to gain a comprehensive understanding of your condition. Always consult with your healthcare provider if you have concerns or questions about your vital signs.
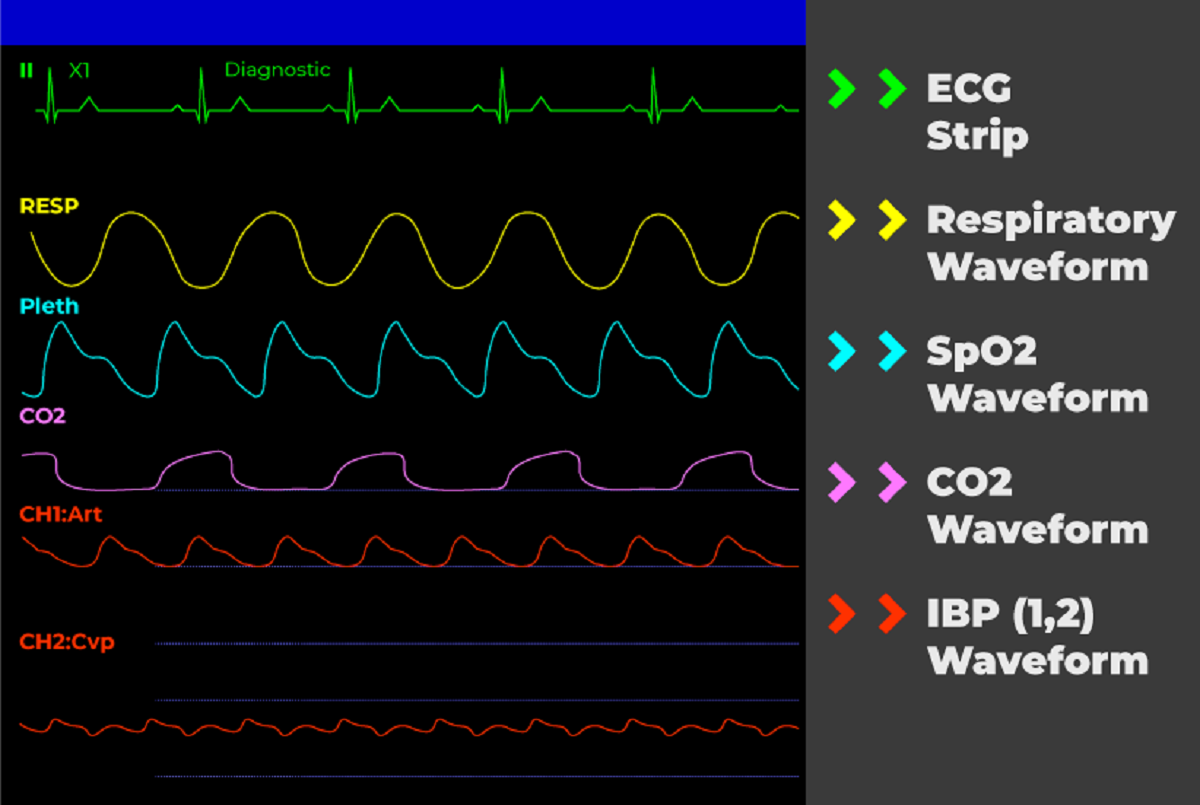
Interpreting EKG Waveforms
Electrocardiogram (EKG) waveforms provide crucial information about the electrical activity of the heart. By understanding how to interpret these waveforms on a hospital monitor, healthcare professionals can assess the heart’s rhythm and detect any abnormalities. Here are some key aspects to consider when interpreting EKG waveforms:
- P Wave: The P wave represents the electrical activity originating from the atria (the upper chambers of the heart). It indicates the contraction of the atria and should appear upright and rounded.
- PR Interval: The PR interval is the time it takes for the electrical impulse to travel from the atria to the ventricles. It should typically be between 0.12 and 0.20 seconds.
- QRS Complex: The QRS complex represents the electrical activity that causes the ventricles (the lower chambers of the heart) to contract. It should typically be less than 0.12 seconds and appear as a narrow, spiked waveform.
- ST Segment: The ST segment represents the period between ventricular depolarization (contraction) and repolarization (relaxation). It should be a straight line positioned at the baseline.
- T Wave: The T wave represents the ventricular repolarization. It should typically be upright, rounded, and slightly asymmetrical.
By analyzing these components of an EKG waveform, healthcare professionals can identify various cardiac conditions, such as atrial fibrillation, ventricular tachycardia, or myocardial ischemia. Abnormalities in the shape, duration, or height of the waveforms may indicate underlying heart problems and require further evaluation and treatment.
It is important to note that interpreting EKG waveforms requires specialized knowledge and expertise. While this overview provides a general understanding, it is not a substitute for professional medical training. Always consult with a qualified healthcare professional for accurate interpretation and diagnosis.
Understanding the basics of EKG waveforms can empower patients to actively engage in discussions about their heart health. By asking questions and seeking clarification from healthcare providers, patients can gain a better understanding of their condition and the recommended treatment options. This collaboration between patients and medical professionals is crucial for ensuring optimal heart health and well-being.
Analyzing Blood Pressure Readings
Blood pressure readings provide important information about the force exerted by blood against the walls of your arteries. Analyzing these readings can offer valuable insights into your cardiovascular health and help healthcare professionals detect and manage conditions such as hypertension. Here’s what you need to know when interpreting blood pressure readings:
When blood pressure is measured, it is typically expressed as two numbers, such as 120/80 mmHg. The top number, known as systolic pressure, represents the pressure in your arteries when your heart contracts and pumps blood. The bottom number, known as diastolic pressure, represents the pressure in your arteries when your heart is at rest between beats.
Normal blood pressure is often considered to be around 120/80 mmHg. However, it is essential to note that optimal blood pressure can vary depending on factors like age and overall health. Blood pressure readings are typically categorized as follows:
- Normal Blood Pressure: A reading below 120/80 mmHg is usually considered within the normal range for adults.
- Elevated Blood Pressure: Readings between 120-129/less than 80 mmHg indicate elevated blood pressure, which may increase the risk of developing hypertension in the future.
- Hypertension Stage 1: Blood pressure readings ranging from 130-139/80-89 mmHg indicate stage 1 hypertension, which signifies high blood pressure and may require lifestyle modifications or medication.
- Hypertension Stage 2: Readings of 140/90 mmHg or higher are categorized as stage 2 hypertension, requiring prompt medical attention and potential intervention.
- Hypertensive Crisis: Extremely high blood pressure readings of 180/120 mmHg or higher may require immediate medical intervention.
Analyzing blood pressure readings helps healthcare professionals determine the risk of cardiovascular diseases and guide treatment decisions. Regular monitoring of blood pressure can help individuals manage their health effectively and make necessary lifestyle changes to prevent complications.
It is crucial to note that blood pressure readings can vary throughout the day due to factors like stress, physical activity, and medications. Therefore, it is essential to monitor blood pressure consistently to obtain accurate and reliable readings.
Understanding and analyzing blood pressure readings empowers individuals to take an active role in their cardiovascular health. By making lifestyle modifications, seeking medical advice, and adhering to prescribed treatments, individuals can maintain healthy blood pressure levels and reduce the risk of heart disease and related complications.
Decoding Oxygen Saturation Levels
Oxygen saturation levels, often measured using a pulse oximeter, indicate the amount of oxygen in your blood. Monitoring and interpreting oxygen saturation levels are crucial for healthcare professionals to assess respiratory function and ensure your body receives an adequate oxygen supply. Here’s what you need to know when decoding oxygen saturation levels:
Oxygen saturation is expressed as a percentage and indicates the proportion of hemoglobin in your blood that is saturated with oxygen. A normal oxygen saturation level is typically between 95% and 100%. Levels below 90% may indicate hypoxemia, a condition characterized by insufficient levels of oxygen in the blood.
Pulse oximeters use infrared light to measure oxygen saturation levels by detecting the differences in absorption of light between oxygenated and deoxygenated blood. The device is commonly placed on a fingertip, earlobe, or toe, and the reading is displayed on the monitor.
Interpreting oxygen saturation levels is vital in various situations, such as assessing lung function, monitoring individuals with respiratory conditions like asthma or chronic obstructive pulmonary disease (COPD), and evaluating critical care patients. It can also aid in determining the need for supplemental oxygen or adjusting ventilator settings.
It is important to remember that oxygen saturation levels may vary based on several factors, including altitude, body temperature, and certain medical conditions. Additionally, individuals with darker skin pigmentation may experience slight measurement variations due to light absorption differences.
Understanding and decoding oxygen saturation levels can help individuals and healthcare professionals track respiratory health and intervene if oxygen levels are below the normal range. Regular monitoring of oxygen saturation levels is especially important for individuals with respiratory conditions or those recovering from surgery or critical illness.
If you receive readings outside the normal range or have concerns about your oxygen saturation levels, it is essential to consult with a healthcare professional for specific guidance and appropriate management.
By decoding oxygen saturation levels, individuals and healthcare providers can ensure that the body is receiving the necessary oxygen supply for optimal functioning and provide timely interventions when needed.
Interpreting Heart Rate and Rhythm
When reading a hospital monitor, one of the essential aspects to consider is the heart rate and rhythm displayed. Monitoring and interpreting these parameters provide valuable insights into the functioning of the cardiovascular system. Here’s what you need to know when interpreting heart rate and rhythm:
The heart rate refers to the number of times the heart beats per minute. A normal resting heart rate for adults typically ranges from 60 to 100 beats per minute. However, it is important to note that factors such as age, fitness level, and underlying medical conditions can influence the heart rate.
Abnormalities in heart rate can indicate various conditions. Bradycardia refers to a heart rate below 60 beats per minute, while tachycardia is a heart rate exceeding 100 beats per minute. Monitoring heart rate can help healthcare professionals identify abnormalities and track the effectiveness of interventions or treatments.
In addition to heart rate, assessing the rhythm of the heart is equally important. The heart rhythm refers to the pattern of electrical impulses that regulate the heart’s contractions. It is typically represented as a sinus rhythm, which indicates a regular and coordinated pattern.
Arrhythmias, on the other hand, represent irregular or abnormal heart rhythms. They can include conditions such as atrial fibrillation, where the atria (upper chambers of the heart) beat irregularly, or ventricular fibrillation, a life-threatening condition characterized by erratic and ineffective ventricular (lower chamber) contractions.
Interpreting heart rate and rhythm on the hospital monitor allows healthcare professionals to detect abnormalities, determine the severity of the condition, and provide appropriate interventions. This can include administering medications to regulate heart rate, performing cardioversion to restore normal rhythm, or recommending further diagnostic tests.
Understanding and interpreting heart rate and rhythm empowers individuals to monitor their cardiovascular health and seek appropriate medical attention when necessary. It is important to remember that while heart rate and rhythm can offer insights into cardiovascular health, they should be assessed alongside other clinical information to make accurate diagnoses and treatment decisions.
If you have concerns about your heart rate or experience symptoms such as palpitations, dizziness, or shortness of breath, it is crucial to consult with a healthcare professional for proper evaluation and guidance.
By interpreting heart rate and rhythm, healthcare providers can assess cardiac function, identify abnormalities, and provide timely interventions to ensure optimal cardiovascular health and well-being.
Understanding Respiratory Rate and Waveforms
In addition to heart rate and rhythm, monitoring respiratory rate is another vital aspect assessed on a hospital monitor. The respiratory rate represents the number of breaths a person takes per minute. Understanding and analyzing respiratory rate and waveforms provide valuable insights into lung function and overall respiratory health. Here’s what you need to know:
Normal respiratory rates vary depending on factors such as age, activity level, and overall health. For adults, the average resting respiratory rate typically ranges from 12 to 20 breaths per minute.
Interpreting the waveform pattern, such as on a capnography monitor, can also provide valuable information about ventilation and the movement of carbon dioxide (CO2) in and out of the lungs. In a healthy individual, the waveform should display a consistent and smooth pattern.
Respiratory rates that are too high, known as tachypnea, may indicate conditions such as respiratory distress, fever, or metabolic imbalance. On the other hand, respiratory rates that are too low, known as bradypnea, may suggest respiratory depression or issues with the central nervous system.
Waveforms, such as those displayed on a capnography monitor, can help assess the efficiency of ventilation and detect abnormalities. A capnography waveform commonly shows the partial pressure of CO2 (end-tidal carbon dioxide or EtCO2) throughout the respiratory cycle. The pattern can provide insights into the adequacy of breathing, the presence of respiratory obstructions, and the effectiveness of interventions such as ventilation support or CPR compressions.
Understanding and interpreting respiratory rate and waveforms aid healthcare professionals in assessing lung function and respiratory health. It allows them to detect abnormalities, monitor response to treatments, and make timely interventions to optimize oxygenation and ventilation.
If you notice changes in your respiratory rate, experience shortness of breath, or have concerns about your lung function, it is crucial to consult with a healthcare professional for proper evaluation and guidance.
Regular monitoring of respiratory rate and waveform patterns is vital for individuals with chronic respiratory conditions, recovering from surgeries, or requiring mechanical ventilatory support. This helps ensure optimal respiratory function and early detection of any changes or complications.
By understanding and analyzing respiratory rate and waveforms, healthcare providers can assess lung function, identify abnormalities, and provide appropriate interventions to maintain respiratory health and well-being.
Reading CO2 Monitor
A CO2 monitor, also known as a capnography monitor, provides information about the levels of carbon dioxide (CO2) in a person’s breath. This measurement is crucial for monitoring respiratory function and evaluating the adequacy of ventilation. Here’s what you need to know when reading a CO2 monitor:
Capnography measures the partial pressure of CO2 during the respiratory cycle and displays it as a waveform. This waveform provides insights into the patient’s ventilation status, the efficiency of exhaled CO2 elimination, and the overall respiratory health.
When interpreting a CO2 monitor, look for the following key parameters:
- Baseline: The baseline represents the beginning of the exhalation phase on the waveform. It indicates the level of CO2 in the patient’s breath when no exhalation is occurring.
- End-Tidal CO2 (EtCO2): EtCO2 represents the maximum level of CO2 in the patient’s breath at the end of exhalation. It indicates the level of CO2 that is being eliminated from the lungs during normal breathing.
- Waveform Shape: The waveform shape on the CO2 monitor should be consistent and exhibit a smooth pattern. Any irregularities or abnormalities in the waveform may indicate issues with ventilation or respiratory function.
- Capnogram: The capnogram is the graphical representation of the CO2 waveform. It helps visualize changes in CO2 levels over time and can provide insights into the efficiency of ventilation and the presence of obstructions.
Interpreting the readings on a CO2 monitor helps healthcare professionals evaluate airway patency, monitor the effectiveness of ventilation support, and detect respiratory abnormalities such as hypoventilation, hyperventilation, or airway obstruction.
It is important to note that a CO2 monitor should be used in conjunction with other clinical assessments to gain a comprehensive understanding of a patient’s respiratory status. Factors such as metabolic conditions, lung diseases, and certain medications can influence CO2 levels, and individual patient characteristics should be taken into account when interpreting the readings.
If you have concerns about the readings on a CO2 monitor or experience symptoms such as shortness of breath or respiratory distress, it is crucial to consult with a healthcare professional for proper evaluation and guidance.
Reading a CO2 monitor allows healthcare providers to assess respiratory function, monitor ventilation support, and make timely interventions to ensure optimal patient care and respiratory health.
Analyzing Temperature Readings
Temperature readings provide valuable information about a person’s body temperature, which is an essential indicator of their overall health. Analyzing temperature readings can help detect fever, monitor response to treatments, and guide appropriate interventions. Here’s what you need to know when interpreting temperature readings:
Temperature can be measured using various methods, including oral, rectal, ear, forehead, or armpit thermometers. The normal body temperature typically ranges between 97.8°F (36.5°C) and 99°F (37.2°C). However, it is important to consider individual variations and factors such as age, time of day, and physical activity.
Interpreting temperature readings involves recognizing deviations from the normal range:
- Fever: A temperature reading above 100.4°F (38°C) is generally considered a sign of fever. Fever often indicates an underlying infection or inflammatory response in the body.
- Hypothermia: When the body temperature drops below 95°F (35°C), it is classified as hypothermia. Hypothermia can occur due to prolonged exposure to cold environments or certain medical conditions.
It is important to note that certain factors, such as physical activity, recent food or fluid intake, and menstrual cycle, can temporarily affect temperature readings. Additionally, different temperature measurement sites may yield slightly different results.
Analyzing temperature readings helps healthcare professionals assess the severity of infections, monitor response to treatments, and guide interventions. Depending on the individual’s condition, management may include medications to reduce fever, fluid intake to prevent dehydration, or external warming techniques to treat hypothermia.
If you have concerns about your temperature reading or experience symptoms such as chills, sweating, or persistent fever, it is important to consult with a healthcare professional for proper evaluation and guidance.
By analyzing temperature readings, healthcare providers can gain insights into a person’s health status, identify potential underlying conditions, and provide appropriate interventions to restore optimal body temperature and overall well-being.
Reading Alert and Alarm Notifications
In a hospital setting, alert and alarm notifications play a crucial role in monitoring patient health and ensuring timely interventions when necessary. These notifications are designed to alert healthcare professionals to potential issues that require immediate attention. Understanding how to read and respond to alert and alarm notifications is vital for providing prompt and appropriate patient care. Here’s what you need to know:
Alert notifications are typically used to provide healthcare providers with important information, such as medication reminders or patient status updates. These notifications are often less urgent, allowing healthcare professionals to review the information and take appropriate action based on their clinical judgement.
Alarm notifications, on the other hand, indicate a significant change or potential danger that requires immediate attention. These alarms are triggered by monitored parameters, such as heart rate, oxygen saturation, or blood pressure, falling outside predetermined thresholds.
Reading alert and alarm notifications involves considering the following factors:
- Severity: Alert and alarm notifications are often categorized into different levels of severity, indicating the urgency of the situation. Healthcare professionals must prioritize their response based on the severity level assigned to the alert or alarm.
- Context: Understanding the patient’s clinical condition and the specific circumstances surrounding the alert or alarm is essential for accurate interpretation and appropriate response. It is crucial to consider the patient’s medical history, current medications, and any recent procedures or interventions.
- Collaboration: Communication and collaboration among healthcare providers are vital when responding to alerts and alarms. Teamwork and effective information sharing help ensure that appropriate actions are taken in a timely manner.
It is important for healthcare professionals to promptly acknowledge alert and alarm notifications and provide the necessary interventions or escalate the situation if needed. Timely responses can help prevent adverse events and minimize potential patient harm.
However, it is equally important to be aware of alarm fatigue, which can occur when healthcare providers are exposed to a high volume of alarms, leading to desensitization and decreased response to alarms. Efforts should be made to streamline alarm systems, prioritize alarm settings, and develop strategies to avoid alarm fatigue while ensuring patient safety.
Regular training, education, and evaluation are essential for healthcare professionals to stay updated on the latest alert and alarm protocols, understand their institution’s specific alarm management policies, and ensure their competency in interpreting and responding to notifications.
By understanding and effectively responding to alert and alarm notifications, healthcare providers can enhance patient safety, reduce adverse events, and provide the highest quality of care to their patients.
Conclusion
Reading and understanding hospital monitors can seem like a daunting task, especially if you are unfamiliar with medical terminology and equipment. However, by familiarizing yourself with the basics, you can gain confidence in interpreting vital signs, waveforms, and other important measurements.
In this guide, we explored the fundamental aspects of reading hospital monitors. We discussed how to interpret vital signs such as blood pressure, heart rate, and respiratory rate. We also delved into the intricacies of reading EKG waveforms, CO2 monitors, oxygen saturation levels, and temperature readings. Additionally, we touched upon the significance of reading alert and alarm notifications to ensure timely interventions.
It is crucial to remember that while this guide provides valuable insights, it is not a substitute for professional medical advice. Always consult with healthcare professionals for accurate diagnosis, interpretation, and treatment.
By empowering ourselves with knowledge about reading hospital monitors, we can actively engage in discussions about our health, understand our conditions better, and collaborate with medical professionals for optimal care. It allows us to take charge of our well-being and make informed decisions regarding our health.
Regular monitoring, accurate interpretation, and prompt response to hospital monitor readings are essential for ensuring comprehensive and timely patient care. Healthcare professionals continuously update their knowledge and skills to appropriately interpret monitor data and provide appropriate interventions for their patients.
Remember, the insights provided in this guide are not exhaustive, and each hospital monitor may have specific features and considerations. Ongoing education, training, and collaboration among healthcare professionals are crucial in navigating the complexities of hospital monitor readings.
By understanding and interpreting hospital monitor readings, we can contribute to the safety, well-being, and improved outcomes of patients in healthcare settings. Together, we can harness the power of knowledge to enhance healthcare delivery and promote optimal health for all.